Hormonal Symptoms in Your 30s: Is It Perimenopause or Under-Eating?
Are you in your 30s and suddenly dealing with fatigue, brain fog, or menstrual changes? You might be wondering if it’s perimenopause or something else entirely.
Shifting hormones can create difficult-to-interpret symptoms at any stage of life. Fatigue, mood changes, joint pain, hot flashes, and menstrual cycle changes are commonly associated with the transition into menopause, also known as perimenopause, but they can occur in women of reproductive age, too.
In fact, under-eating, over-exercising, and stress can all be underlying factors in hormonal shifts and even declining hormone levels. Unfortunately, these factors are not often considered by healthcare professionals, and women presenting with the aforementioned symptoms are sometimes brushed off as perimenopausal. Though it’s possible to begin the transition into menopause in your 30s, it’s important that young women receive proper assessment to rule out other contributors to hormonal shifts.
Estrogen’s Role in Women’s Health and the Risks of Early Menopause
Menopause is the natural end of menstrual cycles caused by declining ovarian hormones. Though a number of hormones are affected by menopause, including progesterone and testosterone, the most notable is estrogen, specifically estradiol. Estradiol is the primary form of estrogen before menopause, and it plays important roles in heart health, bone density, muscle function, and metabolism. Even the mitochondria, which are responsible for producing cellular energy, benefit from estradiol. During the perimenopausal transition, estradiol levels can fluctuate before gradually lowering over time, reaching low but stable levels post-menopause.
Given the many physiological benefits and protective roles of estradiol, it should cause some concern when a woman in her early 30s starts experiencing symptoms of perimenopause, which would indicate a decline of the endocrine system and, inevitably, estradiol. It’s worth mentioning that premature menopause, which occurs in women under 40 years of age, is quite uncommon, occurring in only 1.7% of US women. Additionally, it’s estimated that only 5% of women undergo early menopause, occurring between the ages of 40-45 years. Unfortunately, premature or early menopause carries health risks and is associated with cardiovascular disease, osteoporosis, cognitive impairment, and mood disorders.
What Recent Research Says About Perimenopause Trends for Women in Their 30s
Perimenopause spans the 5-10 years leading up to the final menstrual period, which occurs at approximately 51 years of age in US women. Nonetheless, a recent survey of more than 4,400 women (>30 years of age) highlights concerning trends:
Women in their early 30s are experiencing high rates of moderate to severe perimenopausal symptoms.
More than half of the respondents in the 30-35 age group fell into the moderate or severe symptom category.
The media buzz on this article is most important here–it has been framed around young women suffering perimenopause in silence. However, I think we can look at this differently.
Perimenopause or Hormonal Imbalance?
Menopause is a natural and inevitable life stage, making it easy for both clinicians and women themselves to dismiss a broad array of symptoms as normal aging.
The challenge is that not only are the hormonal fluctuations associated with perimenopause difficult to capture in lab work, but women also experience a mix of symptoms that can be associated with varying life stages. Perimenopausal women experience both vasomotor symptoms (e.g., hot flashes) associated with menopause and menstrual cycle symptoms associated with the premenopausal period. Other symptoms, such as fatigue and brain fog, affect women in all life stages. Adding to the confusion, research shows that adult women have limited knowledge about menstrual health, including knowledge of reproductive hormones and menstrual cycle length. Unsurprisingly, perimenopause can be a confusing period of time, and symptoms may be misunderstood.
However, labeling young women as perimenopausal too quickly may risk missing the true–and often reversible–causes of endocrine decline in young women.
Under-Eating, Over-Exercising, and Stress: How They Cause Hormonal Imbalance
Under-eating, over-exercising, and stress are all factors that can disrupt the hypothalamus-pituitary-thyroid-adrenal-ovarian (HPTAO) axis, resulting in hormonal changes, irregular or missing menstrual cycles, and symptoms that overlap with menopausal symptoms, such as brain fog or even night sweats.
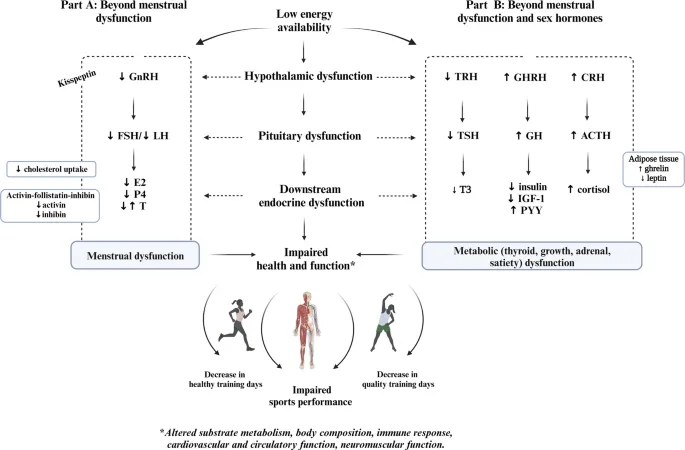
In research, “under-eating” is best described as low energy availability (LEA), which is the mismatch between calories consumed and calories needed by the body to maintain health. The figure below illustrates the hormonal cascade, starting in the hypothalamus, that may occur with LEA in women. These hormonal changes can include low estradiol and luteinizing hormone levels, which may impact ovulation and contribute to irregular or missing menstrual cycles. Other hormonal changes can include low thyroid hormone, low insulin, and high cortisol. These changes can impact metabolism, energy levels, sleep, and your ability to handle stress.
Image Source: Effects of low energy availability on the endocrine system. Ihalainen, J. K., Mikkonen, R. S., Ackerman, K. E., Heikura, I. A., Mjøsund, K., Valtonen, M., & Hackney, A. C. (2024). Beyond Menstrual Dysfunction: Does Altered Endocrine Function Caused by Problematic Low Energy Availability Impair Health and Sports Performance in Female Athletes?. Sports medicine (Auckland, N.Z.), 54(9), 2267–2289. https://doi.org/10.1007/s40279-024-02065-6
With this in mind, it’s important that you receive proper assessment and care when symptoms arise—all of these hormones are important for your overall physical and mental health. Instead of jumping to “perimenopause” when we experience hormonal changes and symptoms, we need to be curious and ask:
Am I eating enough, consistently?
Is my training load appropriate?
Am I handling my stress well?
Am I experiencing nutrient deficiencies or other underlying health issues (e.g., thyroid dysfunction)?
Nutrition and lifestyle are the most powerful levers we have for restoring hormonal health. We need to avoid normalizing symptoms that may, in fact, reflect undernourishment and lifestyle issues–not aging. Even digestive issues that limit the absorption of nutrients and fats can result in hormonal and menstrual cycle changes.
How to Tell If You’re Under-Eating
Under-eating is not just about “feeling hungry.” In fact, many people who chronically under-eat do not feel hungry. This may be due to stress-induced appetite changes or even nutrient deficiencies like iron.
It’s worthwhile to mention that under-eating and inappropriately high training loads are not exclusive to athletes. I often find that those who struggle with under-eating and over-training are those who do not consider themselves an athlete or even athletic. This may be because they’re new to training, don’t take rest days, don’t think they “try hard,” experience high stress levels, or have a busy lifestyle. Such individuals may also feel the effects of diet culture, which promotes foods low in fat, carbohydrates, and calories. Even a high-fiber diet, potentially rooted in a desire to “eat clean,” could interfere with someone’s ability to eat enough food.
Signs You’re Not Eating Enough:
Absent or irregular menstrual cycles
Brain fog
Fatigue
Frequent injuries or illness
Gastrointestinal issues (e.g., constipation and diarrhea)
Increased cravings, especially for sugar or carbohydrates
Lightheadedness
Mood changes, including increased anxiety or depressive symptoms
Poor recovery or training plateaus
Sleep issues like waking in the middle of the night, especially if you wake up hungry
Hormonal Markers to Watch for Under-Eating:
Low estradiol
Low FSH
Low LH
Low TSH
Low active thyroid hormone (T3)
Low insulin
High cortisol
Over time, under-eating and hormonal imbalance in women may result in cardiovascular issues and bone loss, which are also health concerns after the transition into menopause. Identifying under-eating is therefore crucial to maintain health. Some of these hormones can also help differentiate between other root causes of hormonal and menstrual cycle changes. For example, FSH levels increase during menopause, and LH levels typically increase in those with PCOS.
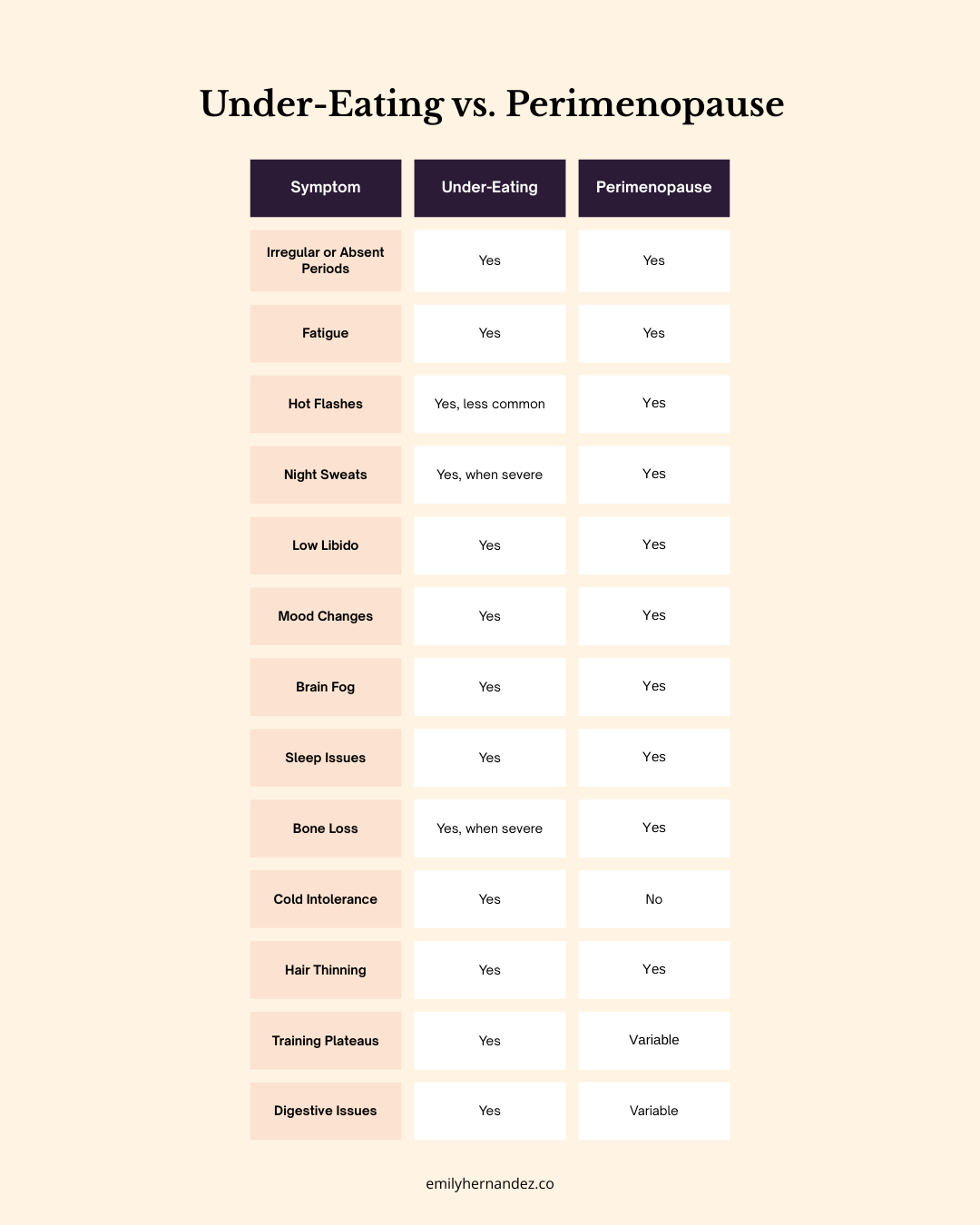
Key Differences: How to Tell If You’re Perimenopausal or Under-Eating
When considering select symptoms of perimenopause, there is considerable overlap with symptoms of under-eating. Keep in mind that symptoms of under-eating may vary based on the severity of the calorie deficit.
It’s recommended that you work with a healthcare provider if you have any of the above health concerns so that you can be properly evaluated. Those experiencing early or premature menopause should seek support from a healthcare provider to identify underlying causes and appropriate treatment options.
Don’t Normalize These Symptoms If It’s Too Soon for Menopause
While perimenopause and under-eating share overlapping symptoms, recognizing the differences allows for better understanding and treatment options of both scenarios. Active women must be especially mindful of fueling properly to support both hormonal health and performance. And most importantly, women will be best supported when their health concerns are not brushed off as a normal part of aging.